Population Health Management (PHM) Software Platforms are enterprise grade digital ecosystems designed to help Healthcare Providers (P2 - Hospitals, Health Systems, ACOs, IPAs, Ambulatory Networks) proactively manage the health outcomes of the defined populations. PHM platforms integrate clinical, operational, and financial data to enable risk stratification, care coordination, quality improvement, and value-based care (VBC) performance.
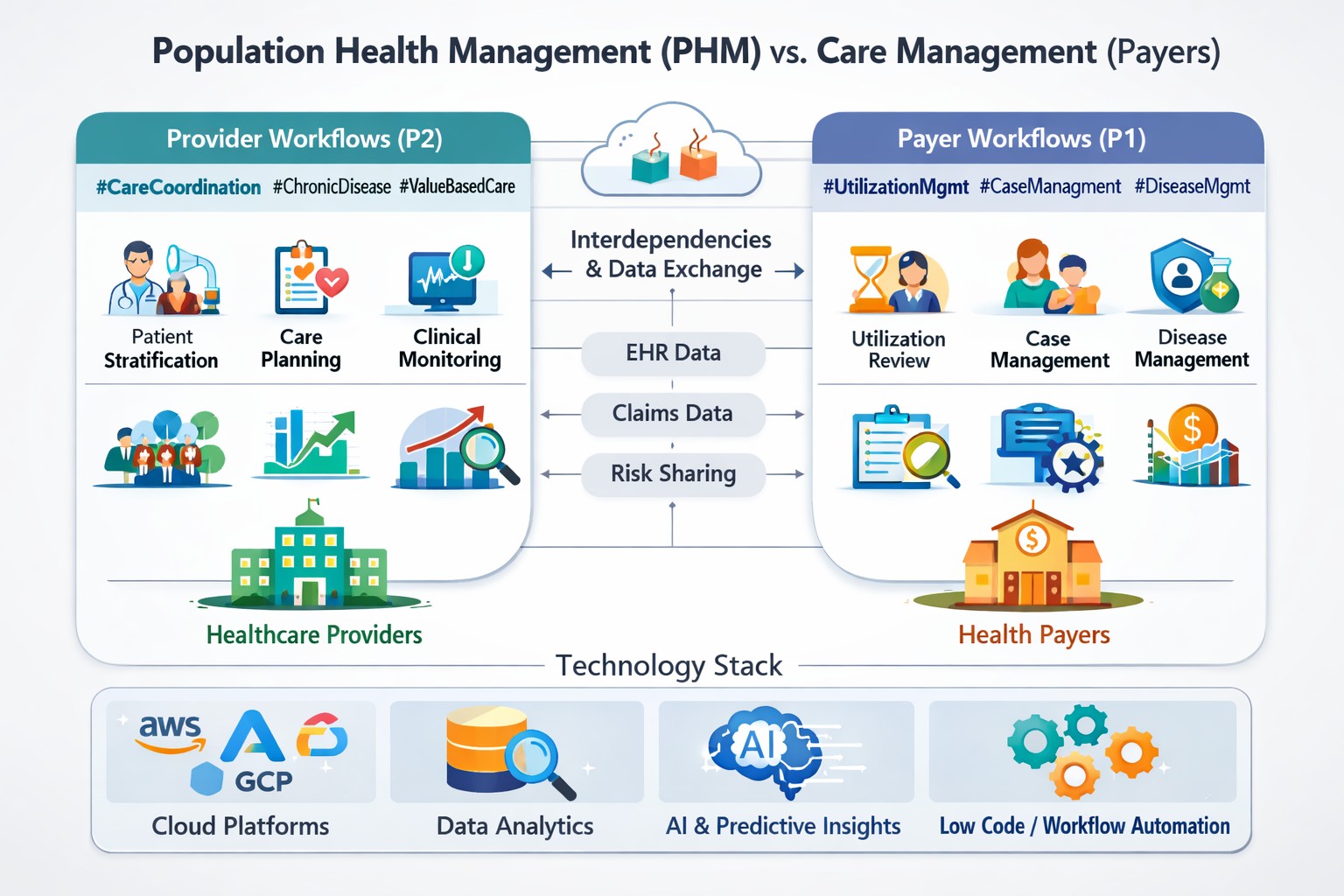
Presenting a comprehensive, technical-cum-business view of PHM workflows from Providers (P2) lens and contrasts them with Payers (P1) Care Management workflows (UM, CM, DM).
Drivers include but not limited to:
• Transition from Fee-for-Service to Value-Based Care (ACO, MSSP, MA, Bundled Payments)
• Rising chronic disease burden and aging populations
• Provider financial risk under shared savings and downside risk models
• Physician burnout and operational inefficiencies
• Demand for real-time, actionable clinical insights
PHM platforms unify data, analytics, workflows, and care orchestration across acute and ambulatory settings.
1. Data Ingestion & Integration
• Sources: EHR (Epic, Cerner), LIS, RIS, Pharmacy, Claims, SDOH, Wearables, HIEs
• Standards: HL7 v2, FHIR APIs, CCD/C-CDA
• Cloud pipelines using AWS Glue, Azure Data Factory, GCP Dataflow
2. Enterprise Data Platform
• Clinical Data Lake (structured + unstructured)
• Enterprise Data Warehouse (Snowflake, BigQuery, Redshift)
• Data governance, MDM, consent management
3. Population Attribution & Registry Management
• Patient attribution (PCP, ACO, Contract-based)
• Disease registries (Diabetes, CHF, COPD, Oncology)
• Cohort definition and segmentation
4. Risk Stratification & Predictive Analytics
• L1: Rule-based risk scoring (HEDIS, CMS, NCQA)
• L2: ML models (readmission risk, gaps-in-care)
• L3: GenAI-driven insights and care recommendations
5. Care Gap Identification
• Preventive care gaps
• Medication adherence gaps
• Post-discharge follow-up gaps
6. Care Coordination & Task Orchestration
• Nurse care managers, social workers, pharmacists
• Automated task routing via BPM engines
• Integration with care plans and referral systems
7. Quality & Outcomes Management
• HEDIS, MIPS, ACO quality measures
• Real-time dashboards for clinicians and leaders
8. Financial & Value-Based Performance Tracking
• Shared savings tracking
• Cost-of-care analytics
• Contract performance benchmarking
Primary focus: Cost containment, compliance, and risk mitigation rather than longitudinal clinical ownership.
1. Utilization Management (UM)
• Prior authorization
• Medical necessity review
• Concurrent and retrospective review
2. Case Management (CM)
• High-risk member identification
• Case management workflows
• Transitions of care
3. Disease Management (DM)
• Condition-specific programs
• Outreach and engagement
• Vendor-driven clinical protocols
PHM for Providers (P2)
• Patient-centric, longitudinal care
• Real-time clinical decision support
• Integrated with EHR workflows
• Revenue + outcomes driven
Care Management for Payers (P1)
• Member centric, episodic
• Claims and authorization driven
• Retrospective and compliance focused
• Cost and utilization driven
• Claims data feeds enrich PHM analytics
• Payer risk scores inform provider care prioritization
• Shared quality measures (HEDIS, Stars)
• Collaborative care plans for high-risk populations
• Value-based contracts act as the binding layer
Data Layer
• AWS, Azure, GCP
• Snowflake, Databricks, BigQuery
Integration
• HL7/FHIR engines
• API gateways
Analytics & AI
• SQL, Spark, MLflow
• Predictive & GenAI models
Workflow & Automation
• BPM, Low-Code (Salesforce, NewgenOne, Pega)
Visualization
• Power BI, Tableau, Looker
Each platform differentiates on data model depth, analytics maturity, workflow integration, and scalability.
• Epic Healthy Planet
• Oracle Health (Cerner HealtheIntent)
• Innovaccer
• Arcadia
• Health Catalyst
• Philips Population Health
• Veradigm
• PHM data product strategy
• Cloud-native architecture design
• EHR and payer data integration
• Agile delivery and platform modernization
• AI-powered care orchestration and analytics acceleration
PHM platforms are no longer optional, they are foundational to Provider success in value-based healthcare. When aligned with Payer Care Management workflows and powered by modern cloud, data, and AI stacks, PHM platforms unlock sustainable outcomes, clinician efficiency, and financial performance.
#PopulationHealthManagement #PHM #ValueBasedCare #HealthcareAnalytics #DigitalHealth #CareCoordination #HealthIT #FHIR #HL7 #CloudHealthcare #AIinHealthcare #GHITDigital