Credentialing in Healthcare: Enabling Trust, Compliance, and Efficiency through Provider Lifecycle Management
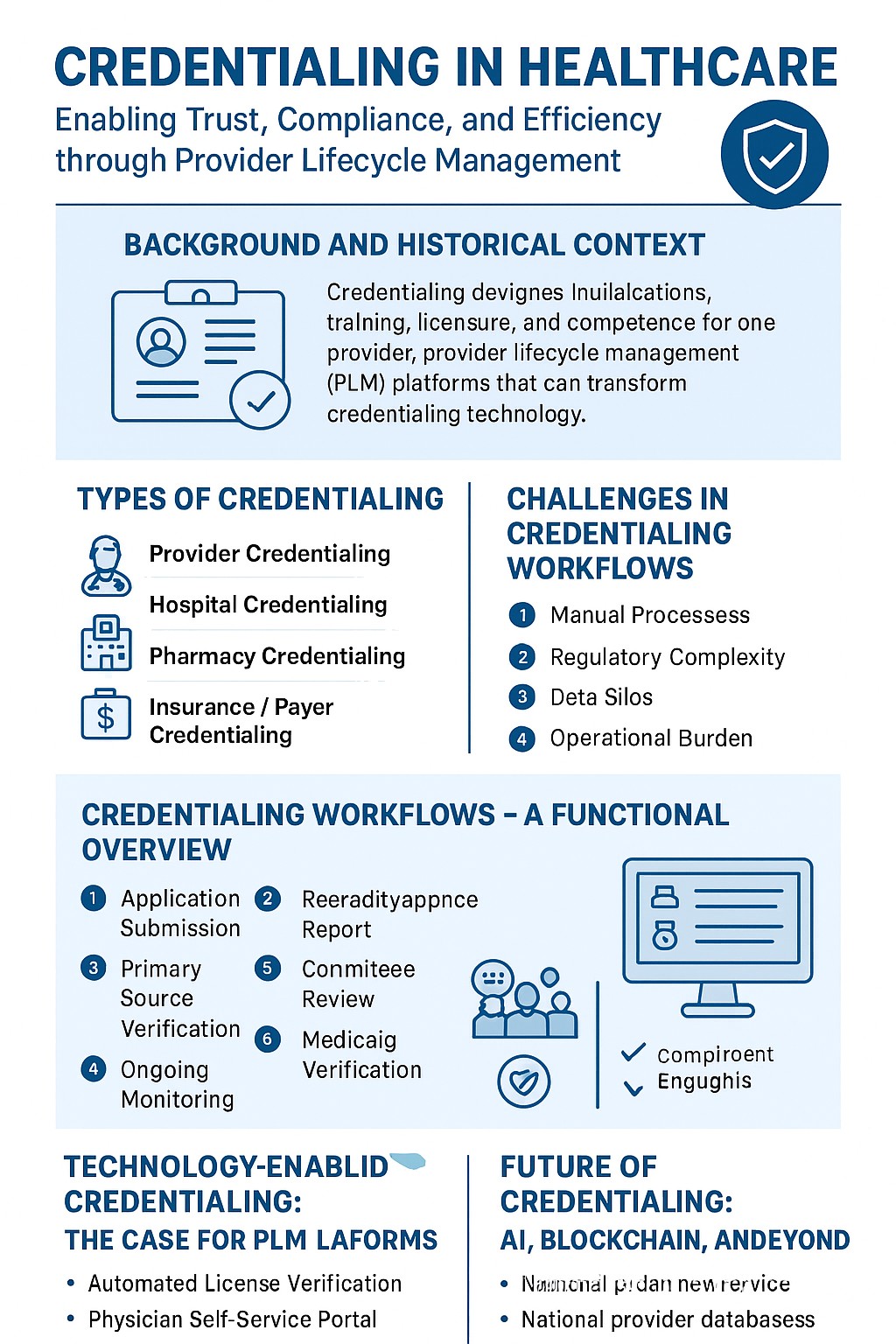
Credentialing in healthcare is the foundational process that validates the qualifications, training, licensure, and competence of providers before they deliver care. In a landscape where patient safety, compliance with federal guidelines (CMS, HHS, HIPAA), and operational efficiency are paramount, effective credentialing is no longer just an administrative requirement—it is a strategic capability. Happy to share the historical context, regulatory frameworks, and challenges of credentialing across provider, hospital, and pharmacy domains. It further highlights how Provider Lifecycle Management (PLM) platforms, powered by low-code automation, AI, and real-time integrations, are transforming credentialing. Credentialing Software Platform streamline license verification, board certification validation, and Medicaid eligibility checks, enabling health systems, payers, and pharmacy networks to ensure compliance, reduce delays, and safeguard patients.
The origins of credentialing date back centuries, when guilds and local medical boards validated physicians through apprenticeships and peer attestations. In the U.S., formalized credentialing took root in the 20th century, driven by the Joint Commission (founded in 1951) and CMS regulations. As healthcare expanded—adding new specialties, complex reimbursement models, and digital care pathways—the scope of credentialing grew from physician qualifications to include pharmacies, advanced practice providers, allied health professionals, and even digital-first telemedicine providers.
Today, credentialing is governed by a combination of:
• Centers for Medicare & Medicaid Services (CMS): Establishing rules for provider enrollment and participation in Medicare/Medicaid programs.
• Department of Health and Human Services (HHS): Overseeing provider participation, fraud prevention, and compliance programs.
• HIPAA & PHI Guidelines: Ensuring that credentialing workflows involving sensitive provider and patient data maintain strict security and privacy safeguards.
• NCQA & URAC Standards: Defining accreditation benchmarks for health plans and credentialing organizations.
Credentialing is not monolithic—it spans across provider categories and service delivery models:
1. Provider Credentialing – Verification of physicians, nurses, and allied health professionals (licenses, certifications, malpractice history, background checks).
2. Hospital Credentialing (Medical Staff Credentialing) – Validation of hospital-employed or affiliated providers through Medical Staff Offices, privileging committees, and peer review boards.
3. Pharmacy Credentialing – Assessment of pharmacists and pharmacy networks, including DEA registration, licensure, and PBM compliance.
4. Insurance / Payer Credentialing – Required for providers to be reimbursed by payers; involves CAQH ProView integrations, NPI validation, and enrollment in payer networks.
5. Telemedicine Credentialing – Emerging area requiring interstate licensure validation (Interstate Medical Licensure Compact), digital practice privileges, and HIPAA alignment.
Credentialing, while critical, is often plagued with inefficiencies:
• Manual Processes: Reliance on spreadsheets, paper submissions, and fragmented portals causes delays (average credentialing time: 60–120 days).
• Regulatory Complexity: Each state board, Medicaid program, and payer has unique verification requirements.
• Data Silos: Provider data is often stored in multiple systems (HR, EHR, payer portals), leading to duplication and inconsistencies.
• Operational Burden: Credentialing coordinators spend disproportionate time chasing documents, verifying licenses, and tracking expirations.
• Compliance Risk: Failure to renew licenses, track sanctions, or verify board certifications can result in penalties, revenue loss, or patient safety risks.
• Provider Experience: Cumbersome processes frustrate physicians and delay onboarding, impacting workforce retention and patient access.
Typical Provider Credentialing Workflow:
1. Application Submission (provider inputs qualifications, licenses, NPI, CAQH updates).
2. Primary Source Verification (licenses, board certifications, malpractice history).
3. Committee Review (credentialing committee/medical staff office approval).
4. Payer Enrollment (integration with CAQH, Medicaid, Medicare, commercial plans).
5. Ongoing Monitoring (license renewals, sanctions checks, DEA re-verifications).
Modern credentialing platforms, ntegrate ECM, BPM, and CCM to orchestrate credentialing seamlessly.
Key Functionalities:
• Automated License Verification – Real-time and scheduled lookups with state boards; tracks expirations with alerts.
• Physician Self-Service Portal – Providers can initiate applications, upload documents, and save progress; dashboard-based progress tracker.
• Credentialing Dashboards & Reporting – Application summaries, expiration trackers, productivity dashboards; low-code configurability.
• Board Certification Verification – Integrates with recognized verification bodies, logs evidence for audits.
• Medicaid Verification – Supports states with structured APIs, uses RPA/manual methods where required.
• HIPAA-Compliant Data Handling – Encryption, access controls, and audit trails ensure PHI security.
The next wave of credentialing modernization will be driven by:
• AI/GenAI: Automating document extraction, anomaly detection, and predictive analytics for renewal trends.
• Blockchain: Creating tamper-proof provider credential registries accessible by payers, hospitals, and regulators.
• National Provider Databases: Expansion of CAQH and NPPES into unified, interoperable platforms.
• Credentialing-as-a-Service (CaaS): Outsourced but API-integrated credentialing utilities for payers and providers.
Credentialing sits at the intersection of compliance, patient safety, and operational efficiency. With regulatory oversight from CMS, HHS, HIPAA, and accreditation bodies, organizations must adopt modern PLM solutions to streamline processes, enhance provider experience, and reduce risks. Credentialing Software Platform Solution demonstrate how automation, low-code configurability, and real-time integrations can transform credentialing into a strategic enabler—reducing onboarding delays, ensuring continuous compliance, and ultimately supporting better patient access to care.
#HealthcareCredentialing, #ProviderCredentialing, #ProviderLifecycleManagement, #HealthcareCompliance, #CMS, #HHS, #HIPAA, #PHI, #HospitalCredentialing, #PharmacyCredentialing, #PayerCredentialing, #MedicaidVerification, #BoardCertification, #HealthcareAutomation, #LowCode, #NewgenONE, #DigitalTransformation, #HealthcareTechnology, #PatientSafety, #CredentialingSolutions